Menopause & Mental Health: Anxiety, Depression, Rage & Brain Fog
Why Mental Health Needs to be at the Centre of Menopause Care
If you’ve entered your 40s or 50s and suddenly feel anxious, overwhelmed, irritable, exhausted, foggy, or simply “not like yourself,” you’re not alone — and nothing about your experience is unusual or unexpected.
What is unusual is that almost no one talks about the profound psychological and emotional impact of menopause.
For decades, menopause has been framed as a collection of physical symptoms:
hot flashes
night sweats
irregular periods
vaginal dryness
But the truth is far more complex — and far more human.
Menopause is a neurological, emotional, cognitive, social, and psychological transition, not just a reproductive one. The hormonal changes influencing your body also influence:
mood
sleep
focus
memory
stress tolerance
confidence
identity
relationships
self-esteem
meaning and purpose
These changes can be destabilizing, confusing, and deeply personal — yet most women are left to navigate them alone, often blaming themselves for symptoms that are biological, predictable, and treatable.
Women tell me every week:
“Why am I so anxious? This isn’t like me.”
“I feel overwhelmed by things I used to handle easily.”
“My brain doesn’t work the same way anymore.”
“I’m snapping more. I don’t recognize myself.”
“I feel lost, like I’m questioning everything.”
These aren’t character flaws. They’re consequences of a shifting internal landscape.
As hormones fluctuate, sleep changes, stress increases, and lifelong roles begin to feel heavier or out of alignment, women experience a kind of psychological ground shift. It is real. It is valid. And it deserves attention.
Mental health is not a side effect of menopause. It is a central part of the transition.
This guide exists because the women I work with aren’t “failing to cope.” They’re moving through a stage of life that affects every dimension of who they are — one that the medical system has historically minimized or overlooked.
You deserve to have your experience named, understood, normalized, and supported. You deserve a framework that makes sense of your symptoms, honours your humanity, and offers a path through this transition that feels grounded and hopeful.
Menopause is not the end of your vitality or emotional wellbeing. It is a powerful inflection point — one that, with support, can lead to deeper clarity, authenticity, and self-understanding than ever before.
This is where we start.
What Menopause Actually Is (and Isn’t)
Many women reach midlife without ever having been taught what menopause truly is — and what it isn’t. Most of what we pick up comes from jokes, stereotypes, or throwaway comments that reduce an entire life stage to hot flashes and mood swings.
Understanding the physiology of menopause is grounding because it makes the emotional and cognitive shifts feel less mysterious — and less personal.
Let’s make it simple.
1. Menopause Is One Day — Literally
Menopause itself is not a stage. It is a single point in time:
→ 12 consecutive months without a menstrual period.
That’s it.
One day.
After that day, you’re considered post-menopausal.
This means most of what women experience — the symptoms, the shifts, the upheaval — is not menopause, but the years leading up to it.
2. Perimenopause Is the Real Transition
Perimenopause is the multi-year process (often 3–10 years) when hormones begin to fluctuate wildly. This is the stage where most symptoms appear.
During perimenopause:
progesterone begins to decline
estrogen starts to swing (not gradually fall)
ovulation becomes inconsistent
cycles shorten, lengthen, or become irregular
the nervous system becomes more reactive
sleep becomes more fragile
stress tolerance drops
cognition is affected
emotional stability changes
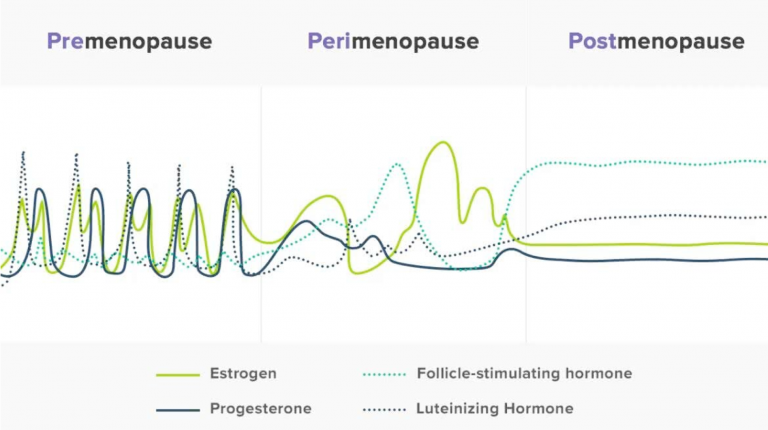
The hormonal chaos of Perimenopause (picture courtesy of Flordis.com.au)
Perimenopause is not subtle — and the psychological impact often appears before physical symptoms are even recognized. Women often notice mood and sleep symptoms before the infamous hot flashes.
3. What Happens After Menopause (“Post-Menopause”)
After that one “menopause day,” hormone levels stabilize at a lower baseline.
Many women expect everything to feel worse after menopause, but the opposite is often true:
anxiety decreases
mood steadies
brain fog improves
sleep becomes more predictable
irritability softens
emotional intensity decreases
Once the hormonal rollercoaster settles, many women feel more grounded and steady than they have in years.
4. Menopause Is Not a Decline — It’s a Recalibration
Culturally, menopause has been framed as the beginning of the end:
“You’re past your prime.”
“Your hormones are drying up.”
“You’re becoming irrelevant.”
None of this is true.
What’s actually happening is:
your hormonal patterns are restructuring
your brain is rebalancing
your nervous system is adjusting
your identity is evolving
Women often emerge from menopause with renewed clarity, energy, and boundaries — not because everything magically gets easier, but because they’ve shed roles, patterns, and expectations that were never sustainable.
5. Your Symptoms Are Not Random — They Aren’t “Just Stress” Either
The emotional, cognitive, and mental-health changes many women experience during perimenopause are directly linked to shifts in hormones, particularly:
progesterone (calming)
estrogen (complex - can be stabilizing and activating)
GABA and serotonin regulation
cortisol reactivity
sleep architecture
This is why:
women who’ve never struggled with anxiety suddenly do
long-managed depression flares
irritability appears without warning
sleep problems explode overnight
brain fog becomes disruptive
self-doubt creeps in
old wounds resurface
These experiences are physiological — not character flaws.
Many women struggle to sort out whether what they’re feeling is anxiety, depression, or hormonal change — I walk through that question here: Is This Anxiety, Depression, or Hormones?.
6. The #1 Thing Women Tell Me:
“I wish someone had told me this earlier.”
Understanding what menopause is — and is not — removes shame.
It restores agency, helps you stop blaming yourself, and it creates space for compassion, support, and choice.
You’re not unraveling.
You’re transitioning.
And transitions — especially ones as complex as this — deserve care, clarity, and context.
Hormones & the Brain: How Shifting Chemistry Shapes Your Mental Health
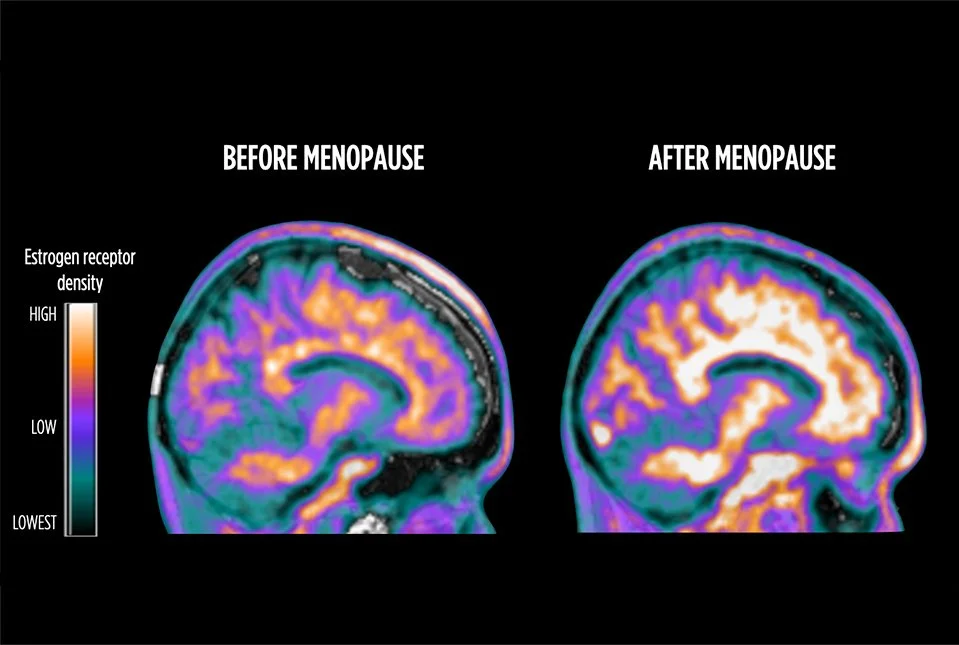
Menopause is often described as a hormonal transition, but what most women aren’t told is that it is also a neurological one. The hormones that fluctuate during perimenopause don’t just affect your cycle — they affect the brain circuits responsible for mood, focus, memory, sleep, stress reactivity, energy, and emotional steadiness. When these hormones change, the brain changes with them.
Understanding this connection can be incredibly grounding. Women often feel immediate relief when they realize, “Oh… it’s not just me. There’s a real reason for this.”
Let’s walk through the major hormonal players in a way that feels clear and manageable.
Progesterone: The Calming Cushion That Begins to Disappear
Progesterone supports the brain’s main calming system: the GABA pathway. When progesterone is steady, women often feel more settled inside, more buffered against stress, and more able to sleep and regulate emotions.
During perimenopause, progesterone is usually the first hormone to decline — and it declines early and steadily. Without it, many women notice they feel more on edge, more easily overwhelmed, more irritable, and less able to access that sense of inner calm they once took for granted. It’s not a personality shift. It’s the loss of a calming influence your brain relied on for decades.
Estrogen: Not “Good” or “Bad,” But Highly Influential
If progesterone is the calming hormone, estrogen is the complex communicator. It influences serotonin (mood), dopamine (motivation and focus), acetylcholine (memory and learning), and even the brain’s blood flow and energy use.
But estrogen doesn’t simply decline in perimenopause — it swings, and sometimes dramatically. These swings can create emotional and cognitive instability that feels unpredictable: a good day followed by a shaky one, or moments where your mood or clarity shift without warning. This isn’t inconsistency in your character — it’s inconsistency in your neurochemistry.
Testosterone: The Quiet Contributor to Motivation and Confidence
Though less talked about, testosterone plays a role in women’s motivation, assertiveness, focus, and even that inner sense of “drive.” Levels naturally decrease with age, and many women begin to feel that drop during perimenopause. The result isn’t dramatic — just a quiet sense of having less spark, less initiative, or less mental momentum than before.
It can feel like losing your “get up and go,” even in areas you used to feel naturally energized.
Cortisol: Why Stress Hits So Much Harder Now
The hormonal shifts of midlife also change how the stress system behaves. Cortisol spikes more easily, emotional recovery takes longer, and the nervous system becomes more reactive. This is why women who have been resilient their entire lives suddenly feel more sensitive to stress or overwhelmed by situations they once handled easily.
You’re not getting “worse” at coping — your brain is simply reacting differently to stressors than it used to, because the hormonal support that once buffered the system has shifted.
Neurotransmitters: The Emotional Messengers Are Also Affected
Because hormones regulate neurotransmitters, changes in estrogen and progesterone ripple out into the systems that control mood, anxiety, sleep, focus, and memory. When these chemical messengers become less predictable, it’s normal to feel:
more anxious or unsettled
more prone to low or flat mood
less motivated
more sensitive or reactive
less able to concentrate or remember things
These are not signs of weakness or aging — they are signs of a brain adjusting to an entirely new hormonal environment.
The Combined Effect: A Nervous System With Less Cushion
When you put all of this together, the nervous system becomes more sensitive, less buffered, and more easily overwhelmed. Things that once felt simple now feel harder. Stressors that once barely registered now hit sharply. Cognitive effort increases. Emotional steadiness decreases.
This doesn’t mean you’re losing resilience — it means your internal supports have shifted.
And Here’s the Good News: The Brain Stabilizes Again
Once you reach post-menopause, hormone levels settle into a more consistent pattern. For many women, emotional intensity softens and cognitive clarity returns. The transition is the turbulent part — not the destination.
You are not declining.
You are recalibrating.
And your brain is doing its best to adapt.
Anxiety in Menopause: Biological, Psychological, and Social Drivers
Anxiety is one of the most common and confusing symptoms of the menopause transition. Even women who have never struggled with anxiety before can suddenly find themselves feeling tense, overwhelmed, restless, or on edge for reasons they can’t quite name. Others who’ve had anxiety in the past may feel it intensify or take on a new shape.
Women often say things like:
“I feel anxious for no reason.”
“My body feels activated all the time.”
“I don’t feel safe, even though nothing is wrong.”
“My mind won’t stop scanning for threats.”
“I wake up in the night with my heart racing.”
This can feel deeply unsettling — especially for women who have always been steady, capable, and grounded. But anxiety in perimenopause is not random, irrational, or a sign that something is “wrong” with you. It has predictable biological roots, psychological layers, and social contributors that make perfect, human sense.
Let’s make sense of all three.
1. The Biological Drivers: A Nervous System Without Its Usual Cushion
Hormones play a central role in how the nervous system regulates anxiety.
Progesterone, the hormone that naturally supports GABA (the brain’s calming system), begins to decline early in perimenopause. Without it, your internal “soothing mechanism” weakens. At the same time, estrogen — which influences serotonin, dopamine, and the stress response — starts fluctuating unpredictably.
The result is a nervous system that has:
less padding
less predictability
less access to calm
a lower threshold for activation
This isn’t psychological anxiety — this is physiological activation. Your body is reacting before your mind even gets a say.
This is why women often describe anxiety that feels like:
a buzzing under the skin
a sense of urgency or doom
heart racing
difficulty breathing deeply
restlessness
nighttime panic
intrusive or looping thoughts
It’s not “in your head.” It’s in your biology.
2. The Psychological Drivers: Why Midlife Brings Old Wounds to the Surface
Biology explains the activation, but psychology explains the content.
Midlife is a phase of reckoning — with identity, relationships, past choices, unmet needs, and long-ignored emotions. Even without hormonal shifts, this is a time when deeper questions rise to the surface:
Am I living the life I want?
Why am I still carrying so much?
What have I tolerated for too long?
What do I actually want now?
Who am I becoming?
When the brain is more sensitive and less buffered, it loses its ability to keep old coping strategies in place: over-functioning, staying busy, suppressing emotions, being the reliable one, prioritizing everyone else.
This creates a perfect storm where:
old anxieties re-emerge,
past traumas feel closer to the surface,
unresolved grief begins to stir,
and the mind feels less able to “hold it together” like it used to.
This isn’t regression — it’s an invitation. Your system is asking you to pay attention.
3. The Social Drivers: The Weight Women Carry in Midlife
If all you were managing was hormonal change, anxiety would still be understandable. But most women at this stage are also holding:
teenagers or young adults needing support
aging parents
midlife relationship strain
high-pressure careers
financial responsibilities
household management
the emotional labour of everyone around them
And on top of that, women often receive absolutely no cultural support, no workplace accommodations, and very little real-world validation of what they’re going through.
Anxiety thrives in conditions of:
responsibility without rest
pressure without support
expectations without relief
You’re not “more anxious” — you’re carrying more than ever with less physiological support than you’ve ever had.
It makes sense that your system feels stretched thin.
4. How Anxiety Feels in Perimenopause (and Why It Feels So Different)
Women who never had difficulty driving are often surprised when it becomes anxiety-provoking in perimenopause.
The anxiety of perimenopause often feels different from earlier-life anxiety. Women describe it as more physical, more unpredictable, and harder to soothe with old strategies. Sometimes it shows up as nighttime surges. Sometimes as panic-like episodes. Sometimes as a constant hum of dread or restlessness.
This is not a sign your anxiety is “getting worse.”
It’s a sign that hormonal instability is changing the way your nervous system responds to stress. The same stressor that barely bothered you five years ago now hits a more sensitive system.
And because women often don’t know this is normal, they interpret the anxiety personally:
“Why can’t I cope anymore?”
“Why am I falling apart?”
“Why is everything so overwhelming?”
But the truth is you’re not falling apart — your internal chemistry is shifting, and your nervous system is trying to adapt.
For many women, anxiety shows up most intensely at night, particularly in the early morning hours, which I explain more fully here: Nighttime Anxiety: Why It Spikes in Midlife & How to Calm Your System.
5. The Most Important Thing to Know
You’re not imagining this.
You’re not being dramatic.
You’re not suddenly “an anxious person.”
You’re not losing resilience.
You’re navigating a biological transition that affects every layer of your emotional and physiological functioning. And you deserve support — real support — while you go through it. This anxiety is explainable and treatable.
Anxiety during perimenopause often feels different than earlier in life — more physical, more sudden, and harder to regulate — which I explore in depth here: Perimenopausal Anxiety vs Generalized Anxiety: How To Tell the Difference.
Depression & Low Mood: When Hormones Mimic or Exacerbate Mood Disorders
Depression during the menopause transition can feel confusing and frightening. Many women who have never struggled with low mood before suddenly find themselves feeling flat, sad, unmotivated, or disconnected from their usual sense of self. Others who have a history of depression may feel old symptoms reappear in ways that feel unfamiliar or harder to manage.
Women often say things like:
“I don’t feel joy the way I used to.”
“Everything feels heavier now.”
“I wake up with a sense of sadness I can’t explain.”
“I feel ungrounded… disconnected from myself.”
“Nothing is wrong, but I’m not okay.”
This can feel alarming, particularly for women who pride themselves on resilience, independence, and emotional strength. But depression in perimenopause is not a personal failing — it is a physiological and psychological response to a system under strain.
Let’s talk about what’s actually happening.
1. The Biological Foundations: Mood Is Chemical Before It Is Cognitive
Estrogen and progesterone influence serotonin, dopamine, and other neurotransmitters that regulate mood, motivation, and emotional steadiness. When these hormones fluctuate or decline, the brain’s usual “mood scaffolding” becomes less consistent.
For some women, this feels like a gentle but persistent flattening — a dampened ability to feel joy, interest, or satisfaction. For others, it feels like sudden drops in mood that come out of nowhere. The key is understanding that the emotional shifts often begin in your physiology.
You’re not choosing sadness.
Your chemistry is changing beneath you.
2. The Psychological Layer: Why Midlife Exposes Old Wounds and Deep Questions
Even without hormonal changes, midlife is a period of immense psychological transition. Women often begin facing questions they’ve postponed for years — about identity, meaning, unmet needs, unsatisfying relationships, lost dreams, or the roles they’ve carried for too long.
At the same time, long-standing coping strategies (over-functioning, staying busy, caretaking, compartmentalizing, striving) start to break down because the system no longer has the internal stability to sustain them.
This combination can produce a type of depression that feels like a quiet calling inward — a sense that the life you’ve built no longer fits in the way it once did.
It’s not failure.
Think of it as an awakening.
3. The Social Context: The Weight of Being “The Reliable One”
Women entering perimenopause are often at the peak of their responsibilities — raising teens or young adults, supporting aging parents, maintaining careers, managing households, absorbing emotional labour, and carrying the invisible load.
At the same time, society offers almost no acknowledgment or accommodation for the emotional and cognitive strain of menopause. Many women feel invisible, misunderstood, or expected to carry on as if nothing has changed.
Depression thrives in environments of high responsibility and low support. What you’re feeling is not personal weakness — it’s structural and cultural.
4. How Depression in Perimenopause Feels (And Why It Feels Different)
Depression during this transition doesn’t always look like what people imagine. Instead of deep sadness, it may show up as emotional numbness, irritability, withdrawal, difficulty feeling joy, or a sense of heaviness in the body.
For some, it feels like grief — but without a clear trigger. For others, it feels like a loss of identity, confidence, or spark.
Many women describe it as:
“I’m here, but I’m not really here.”
“I don’t feel like myself anymore.”
“Everything takes so much effort.”
This is not a sign that you are losing your resilience or your emotional strength. It is a natural response to both internal and external shifts happening at the same time.
Some women don’t experience menopause-related mood changes as sadness, but as emotional flatness or numbness — something I explore here: Depression or Depletion? Understanding Emotional Flatness in Perimenopause.
5. The Most Important Thing to Know
Depression in perimenopause is more common than in pre- or post-menopause, understandable, and treatable. It responds to the same therapeutic and medical supports as depression at any other stage of life — and it also improves as hormones stabilize. You are not “becoming depressed.” You are living inside a nervous system undergoing a profound transition.
And with the right support — emotional, psychological, relational, and sometimes medical — women often emerge from this stage with more clarity, strength, and authenticity than they have ever known.
Some women don’t experience menopause-related mood changes as sadness or anxiety, but as emotional flatness or loss of pleasure — something I explore here: The “Blankness” No One Talks About: Anhedonia in Perimenopause.
Irritability, Anger & Rage: The Neurobiological and Emotional Roots
Irritability — and, for some women, sudden bursts of anger or even rage — is one of the most misunderstood symptoms of the menopause transition. Women often describe themselves as “snapping,” “losing it,” or feeling “uncharacteristically reactive.” Even small irritations can ignite a surprisingly intense internal surge.
Most women don’t talk about this part because they feel ashamed, confused, or frightened by it.
But irritability and rage in perimenopause aren’t about being “moody,” “losing control,” or becoming someone you don’t recognize. They are the natural result of a nervous system stretched thin, depleted of hormonal support, and carrying more emotional labour than ever before.
Let’s break down why this happens — with compassion, honesty, and zero judgment.
1. The Biological Roots: A More Sensitive Stress System
As progesterone declines, women lose a significant buffer against stress. This hormone once provided a sense of internal steadiness — a quiet cushion between stimulus and reaction.
When progesterone is low and estrogen is fluctuating, the stress response system becomes quicker to activate and slower to calm down. This means:
noise feels louder
interruptions feel sharper
demands feel heavier
chaos feels intolerable
So, it’s not that your tolerance has suddenly disappeared. It’s that your nervous system is operating with less insulation. This biological shift alone can make irritability feel like it’s sitting right under your skin, ready to spark.
2. The Psychological Roots: Suppression Has a Shelf Life
Many women reach midlife having spent decades:
accommodating others
tolerating dysfunction
over-functioning
staying quiet to keep the peace
swallowing resentment
prioritizing harmony over authenticity
Perimenopause often brings these patterns to a breaking point. With fewer internal resources and a more sensitive emotional system, women can no longer suppress what they’ve been absorbing.
In therapy, women often say:
“I can’t stuff it down anymore.”
“I’m reacting to things I tolerated for years.”
“I feel like I’ve reached my limit.”
Don’t think of this as regression - it’s honesty emerging after years of containment. The irritability is sometimes less about hormones and more about finally feeling the weight of what you’ve been carrying for decades.
3. The Social Roots: The Cost of Being the Strong One
If women had genuine social safety nets, equitable household labour, supportive workplaces, and permission to rest, irritability wouldn’t spike the way it does.
But many women in midlife are holding:
teenagers with changing needs
partners who assume your stability
aging parents
demanding jobs
financial pressures
the invisible emotional load of the household
Add hormonal vulnerability to a lifetime of being the default caregiver, emotional regulator, and crisis manager — and irritability becomes a predictable response to chronic overload. Your irritability isn’t a flaw; it’s data telling you something about your limits, not your character.
4. The Emotional Roots: Anger as a Signal, Not a Problem
Anger and irritability are among the most disrespected emotions for women. Yet they are often the most informative.
Rage in perimenopause can point to:
needs that have gone unmet
boundaries that have been neglected
roles that no longer fit
relationships that lack reciprocity
exhaustion that has been minimized
patterns that feel unsustainable
Sometimes the anger isn’t about the present moment at all — it’s accumulated from years of absorbing, appeasing, and enduring. In this light, irritability becomes less of a symptom and more of a messenger.
5. You Are Not Becoming an Angry Person — You Are Becoming an Honest Person
This is the sentence women often exhale into.
Midlife ushered in by hormonal change has a way of stripping away the coping strategies that kept everyone else comfortable at your expense. Without the hormonal padding, without the emotional over-functioning, without the energy to pretend, what remains is the truth.
Your irritability is not a sign that you’re losing control, rather, it’s a sign to start listening to yourself. This is a moment for self-compassion, not self-blame.
6. The Good News
As hormones stabilize, the intensity of irritability and rage softens. Women often feel more anchored, more regulated, and more steady again. And when the psychological and social pieces are addressed — boundaries, support, balance, self-expression — irritability often becomes a guide rather than a burden.
You are not “too much.”
You are overwhelmed.
And your nervous system is doing its best in a season that demands more from you than ever before.
With support, this becomes a turning point — not a failing.
Sleep Disruption: Why it Happens & How it Affects Mental Health
Sleep problems are one of the hallmark symptoms of perimenopause. Even women who have slept well their entire lives suddenly find themselves wide awake at 2:00 a.m., tossing and turning, waking drenched in heat, or unable to fall back asleep after the slightest disturbance.
And because sleep is the foundation for emotional regulation, memory, cognitive clarity, and overall resilience, these nighttime disruptions ripple into every corner of a woman’s day.
Women often say:
“I feel like I’m operating on fumes.”
“I wake up at 3 a.m. for no reason — and my mind starts spinning.”
“I feel like a different person now that I’m not sleeping.”
“My anxiety is so much worse when I’m exhausted.”
“I’m irritable because I’m tired, and I’m tired because I’m irritable.”
Sleep changes are not random, and they’re not your fault. They arise from predictable hormonal shifts — and they help explain why emotional and cognitive symptoms soar during this stage.
Let’s explore why sleep becomes so fragile.
Sleep disruption plays a central role in emotional regulation during the menopause transition, shaping anxiety, mood, and resilience — more on that here: Menopause, Sleep, and Mood: How Exhaustion Changes Everything.
Hello 3am.
1. The Big Hormonal Shift: Progesterone Decline
Progesterone plays a surprisingly important role in sleep. It supports GABA, the neurotransmitter that quiets the brain and helps it transition into rest. As progesterone declines — often early in perimenopause — the brain loses some of its natural calming influence.
This is why women often describe feeling:
less relaxed at bedtime
more restless
more easily startled or awakened
unable to “turn off” their minds
It’s not a sleep problem in isolation — it’s a regulation problem.
2. Estrogen’s Instability Disrupts Temperature and Sleep Architecture
Estrogen affects the body’s thermoregulation system as well as the brain pathways that control sleep stages. When estrogen swings, many women experience sudden heat surges, night sweats, or a spike in alertness just as they try to fall or stay asleep.
A single night of disrupted sleep is frustrating.
Months of it become debilitating.
This is one of the biggest reasons midlife anxiety, irritability, overwhelm, and brain fog escalate. The system simply isn’t getting the restoration it needs.
3. Cortisol Becomes More Reactive (Especially at 2:00–4:00 a.m.)
During perimenopause, the stress-response system becomes more sensitive. Cortisol spikes more easily — and those spikes are most likely to occur during the early morning hours.
Women often describe waking with their heart pounding, mind racing, or body feeling “on alert,” even when nothing is wrong. This isn’t panic “out of nowhere.” It’s a biological stress response being triggered during sleep.
Once cortisol rises, falling back asleep becomes incredibly difficult.
4. The Emotional Impact of Long-Term Sleep Loss
Poor sleep doesn’t just make you tired — it changes the emotional landscape of your day.
With ongoing sleep disruption, women may notice:
increased anxiety
lower stress tolerance
irritability or emotional reactivity
difficulty concentrating
reduced resilience
lower mood
more overwhelm
intrusive or catastrophic thinking
hopelessness or despair on particularly bad days
Sleep loss magnifies every other symptom of perimenopause. Even mild hormonal fluctuations feel enormous when your brain has not been restored overnight.
This is why some women say, “Everything feels harder now.”
They’re not imagining it — everything is harder without adequate sleep.
If you’re curious about how these emotional changes evolve as you move into menopause, my mental health guide for postmenopause offers a clear overview of what often stabilizes and what may continue.
5. Why Women Blame Themselves (And Why They Shouldn’t)
Women internalize sleep struggles differently than men. They often blame themselves:
“I must be doing something wrong.”
“I should be able to relax.”
“If I weren’t so stressed, I’d sleep better.”
But this is not a mindset issue. It’s not a lack of discipline, meditation, supplements, or perfect sleep hygiene (although sleep hygiene typically needs tweaking). It is chemistry, not character.
And when women understand this, the self-blame softens — often for the first time.
6. Your Future with Sleep?
One of the most important truths about sleep in midlife is that sleep does not automatically improve once you reach menopause. In fact, research consistently shows that sleep often becomes even more disrupted in postmenopause, especially for women who already had difficulty sleeping during perimenopause.
This isn’t because you’re “doing anything wrong.” It’s because sleep architecture continues to change as hormones settle into their new baseline.
Women in postmenopause commonly report:
lighter, more fragmented sleep
waking up multiple times per night
early morning awakenings
difficulty returning to sleep once awake
persistent nighttime anxiety
continued sensitivity to heat or temperature shifts
This is not a failure of the body — it’s the long-term effect of reduced estrogen and progesterone on the systems that regulate temperature, stress, mood, and sleep depth.
And while this may sound discouraging, here’s the empowering part:
Sleep can still improve — it just doesn’t improve automatically.
With support, treatment, and understanding, sleep can become steadier, deeper, and more restorative again. But it requires attention, not patience.
Many women feel noticeably better with:
targeted therapy (CBT-I, ACT-based strategies)
treating nighttime anxiety or cortisol surges
optimizing sleep environment and routines
medical support, including evaluating whether HRT is appropriate
addressing pain, mood symptoms, and possibly sleep apnea and restless legs
reducing stimulation and cognitive load before bed
So the truth isn’t “sleep goes back to normal.”
The truth is:
Sleep is a long-term area of vulnerability in midlife — and a long-term area where support can make a meaningful difference.
You’re not destined for lifelong exhaustion.
You simply deserve better support than you’ve ever been given.
7. You Deserve Rest, Not Pressure
When women stop blaming themselves and start understanding their biology, something shifts. They see that their exhaustion is not laziness, weakness, or failure — it’s physiology.
You deserve compassion for how hard it is to function without restorative sleep, and support in reclaiming the rest your body is desperately trying to find.
Cognitive Function: Memory, Focus, and Word Retrieval in the Midlife Brain
Cognitive changes in perimenopause are among the most distressing — not because they’re dangerous, but because they are surprising, disruptive, and often feel out of character for women who have always been sharp, capable, and mentally nimble.
Many women say:
“I keep losing my train of thought.”
“My words just… disappear.”
“I used to multitask without thinking. Now it overwhelms me.”
“I feel foggy in a way I can’t explain.”
These experiences can be frightening, especially in a culture that equates cognitive changes with decline. But perimenopausal cognition is not about decline — it’s about instability. Think of it as your brain as recalibrating during a time of hormonal turbulence.
Let’s walk through what’s actually happening.
1. Brain Fog: The Most Misunderstood Symptom of Midlife
Brain fog is not a single symptom — it’s a cluster of experiences that include slower processing, difficulty concentrating, mental “heaviness,” and a sense of cognitive fatigue.
What makes brain fog unique in perimenopause is its inconsistency: you may feel totally clear one day and deeply foggy the next. This variability mirrors the hormonal swings happening under the surface.
Nothing is “wrong” with your intelligence or capacity — your cognitive efforts are being pulled in different directions physiologically.
2. Why Word-Finding Issues Become So Common
Word retrieval relies on stable neural pathways supported by estrogen. Estrogen helps the brain use glucose. When estrogen fluctuates quickly — which it does constantly in perimenopause — these pathways become temporarily less accessible.
Women describe this as knowing the word but not being able to reach it, or losing nouns, names, and familiar terms mid-sentence. This isn’t a memory loss issue — it’s a retrieval delay in a brain working with inconsistent chemical support.
The words are still there.
The path to them is temporarily glitchy.
3. Focus and Attention Change When the Brain Is Overloaded
Perimenopause creates the perfect environment for attention to become strained:
sleep is disrupted
stress is heightened
emotional labour increases
hormonal stability decreases
Even if you’ve always been focused, organized, and efficient, your cognitive bandwidth is now being divided between regulation and everything else. The brain prioritizes survival and stability over sustained concentration. This is why even simple tasks can feel harder, and interruptions feel more jarring.
Midlife attention issues are not “ADHD” appearing out of nowhere — they are the cognitive side effects of a system overwhelmed from the inside.
4. Multitasking Often Feels Impossible — and That Makes Sense
“Multitasking” (really, switching between tasks) depends on the prefrontal cortex, a region that is sensitive to stress, sleep loss, and hormonal shifts. In perimenopause, the prefrontal cortex simply has fewer resources to manage multiple demands at once.
This is why switching between tasks can feel jarring, noise becomes intolerable, and even minor interruptions can lead to cognitive overload. It’s capacity being stretched thin.
Your brain is asking for single-tasking, not because you’re less capable, but because you’re less buffered.
5. Why These Symptoms Can Feel Scary (Even Though They Aren’t Dangerous)
The suddenness of these cognitive shifts — especially for women who have always been mentally sharp — can create fear. Women often quietly worry about dementia, even though perimenopausal cognitive symptoms are:
extremely common
temporary
reversible
unrelated to long-term cognitive decline
The fear arises not from the symptoms themselves but from the lack of information women receive about them.
When women understand the science, their anxiety about their cognition often decreases dramatically.
6. A Key Reassurance: Cognitive Stability Returns
Once hormones settle — naturally or with support — the brain regains its clarity, steadiness, and reliability. Many women describe feeling like they “got themselves back” after menopause.
Cognitive changes are not a sign of who you’re becoming.
They’re a sign of what your brain is navigating right now.
Your wisdom, intelligence, sharpness, and insight remain intact.
7. If You Are Struggling, It Doesn’t Mean You’re Failing
Midlife places extraordinary demands on women — professionally, emotionally, relationally, and cognitively — at the exact moment their nervous systems have the least internal support.
If you’re struggling to think clearly, remember things, or stay focused, you’re not “slipping.” You’re human, you’re overloaded, and you’re navigating a transition that touches every part of who you are.
Identity Shifts: “Who Am I Now?”
One of the most unsettling — and least discussed — parts of the menopause transition is the quiet shift in identity that often happens beneath the surface. It’s not simply a mood change or a cognitive shift. It’s a sense that the internal compass you’ve relied on for decades is recalibrating, and you’re suddenly questioning things that once felt stable.
Women often say:
“I don’t feel like the same person anymore.”
“I’m reevaluating everything.”
“I used to know exactly who I was — now I’m not so sure.”
“I feel like parts of me are waking up, and parts of me are fading.”
This can feel disorienting, even frightening, especially if no one warned you that identity itself can shift in this stage of life. But this experience is not a crisis — it’s a transition. A profound and meaningful one.
Here’s why this happens.
1. Hormonal Changes Don’t Just Affect Mood — They Affect Self-Perception
Estrogen, progesterone, and testosterone have subtle but powerful influences on confidence, clarity, emotional regulation, and a sense of internal stability. When these hormones fluctuate or decline, many women experience moments of self-doubt or internal shakiness that feel like, “Who even am I right now?”
This is a temporary blurring of the edges while the brain and nervous system adapt to a new internal landscape. Like standing on shifting ground, not because your foundation is weak, but because the terrain is changing.
2. The Roles You’ve Performed for Decades Start to Feel Different
Midlife is often the first time women have the emotional space — or the forced pause — to examine the roles they’ve played for years:
the caregiver
the over-functioner
the stabilizer
the emotional anchor
the high achiever
the peacekeeper
the “strong one”
the dependable one
For many women, these roles once felt aligned, or at least manageable. But as hormones shift, sleep disrupts, and tolerance for self-abandonment fades, these roles start to feel heavy, restrictive, or even incompatible with who they’re becoming.
A truth that many women feel but rarely say aloud:
“I’m tired of being the person everyone expects me to be.”
This is not selfishness. It’s awakening.
3. Emotional Bandwidth Shrinks — And Insight Expands
When your nervous system has less buffer, you stop being able to perform or pretend your way through misalignment. You may find you no longer have the energy to tolerate:
drained relationships
imbalanced workloads
invisible labour
environments that never gave enough back
the constant prioritizing of everyone else’s needs
the emotional weight you used to carry silently
What looks like irritability or frustration on the surface is often clarity underneath. You’re no longer willing to stretch yourself to keep systems running that were built on your self-sacrifice.
This is why midlife often brings abrupt insight:
“I don’t want to do this anymore.”
“This is no longer enough.”
“I need more support.”
“I want something different now.”
Insight grows as tolerance shrinks — not because you’re becoming less resilient, but because you’re becoming more honest.
4. Old Dreams, Needs, and Parts of Self Resurface
As the brain and body shift, women often reconnect with parts of themselves that went quiet during the decades of caretaking, career-building, partnering, and raising families.
You may notice:
creative impulses resurfacing
a desire for solitude
curiosity about different career paths
questioning long-term relationship patterns
longing for deeper meaning
grief for the parts of life you put on hold
a quiet hunger for authenticity
These longings aren’t new — they’ve just been waiting for space. Midlife gives you that space, not by choice but by necessity. The system says:
“Something is changing. Pay attention.”
5. This Isn’t an Identity Crisis — It’s an Identity Expansion
The narrative that women in midlife are “falling apart,” “becoming emotional,” or “going through a crisis” is deeply rooted in sexism and misunderstanding.
What’s actually happening is this:
Your sense of self is updating.
Your values are shifting.
Your capacity is informing your boundaries.
Your intuition is growing louder.
Your needs are stepping forward.
Your life is asking to be aligned — not maintained.
Think of it as midlife helping to reveal the actual you.
6. The Most Important Thing to Know
The discomfort you feel is not a sign of decline — it is a sign of emergence. You are stepping into a version of yourself shaped not by who you were expected to be, but by who you finally have permission to be.
And you deserve support, compassion, and clarity as you grow into the next chapter of your life — with more wisdom, honesty, and self-understanding than ever before.
Stress, Burnout & Emotional Labour: The Invisible Load That Magnifies Symptoms
By the time women reach midlife, they are often operating at a level of sustained stress that would overwhelm anyone — but they’ve adapted to it so gradually that it feels normal. The constant multitasking, caregiving, coordinating, smoothing, anticipating, absorbing, and holding everyone else’s needs creates a baseline of emotional strain that most women don’t even recognize as stress anymore.
Then perimenopause arrives, and the system that once carried all of this begins to falter.
Women often tell me:
“I handled more than this five years ago. Why does everything feel harder now?”
“I’m exhausted in a way I can’t explain.”
“Nothing changed — yet everything feels heavier.”
That last sentence is the most revealing.
Often, nothing external changed.
But everything inside did.
Let’s explore why the emotional load of midlife hits differently — and why burnout is so common during this transition.
1. Chronic Stress Becomes “Invisible Stress”
When women spend decades functioning at high capacity, their stress becomes so normalized that they stop feeling it consciously. They move through the world with a level of tension and vigilance that feels like second nature.
But chronic stress reshapes the nervous system.
It changes how quickly cortisol rises, how long it stays elevated, and how much recovery time the body needs. By midlife, the system is often depleted, even if the woman herself feels like she’s “used to it.”
Perimenopause then lowers the threshold even further. A stress level you once managed without thinking now registers as too much.
Nothing about this is about willpower.
It’s physiology meeting accumulated load.
2. Emotional Labour Intensifies With Age — But Women’s Bandwidth Shrinks
The emotional labour women carry — the subtle, constant management of other people’s feelings, needs, conflicts, expectations, and wellbeing — does not decrease as they age. If anything, it increases.
Midlife is often the point where women are:
supporting aging parents
managing teenage or young adult children
holding the emotional climate of their household
navigating changing relationships
maintaining careers under pressure
providing unseen support to partners
making decisions for everyone else
serving as the glue for extended family
While all of this is happening, perimenopause reduces a woman’s internal resources. Her sleep is lighter. Her nervous system is more reactive. Her tolerance for noise, chaos, and interruption shrinks. Her ability to suppress her own needs decreases.
The math simply stops adding up.
Even if the responsibilities stay the same, the cost of carrying them increases.
Yes, in perimenopause, 2+2 does in fact = 5.
3. Burnout Isn’t Sudden — It Accumulates Quietly
Most women don’t burn out because something dramatic happens. They burn out because they’ve been running at 120% for so long that the drop in hormonal support brings the truth into focus.
The signs often appear gradually:
tasks requiring more effort
more irritability or emotional fatigue
feeling chronically overstimulated
reduced patience
a sense of heaviness or dread
difficulty making decisions
withdrawing from social roles
feeling “checked out” or numb
Women often interpret this as personal failure or aging, but it’s the body’s way of saying: “I’ve done too much for too long.”
Burnout in midlife is more like erosion than collapse.
4. Why Midlife Stress Feels More Personal
Perimenopause doesn’t just reduce internal capacity — it increases emotional sensitivity. Women begin to notice the inequities, imbalances, and invisible burdens they once tolerated. Their insight sharpens, while their ability to carry injustice weakens.
This creates a perfect storm:
things that were quietly tolerated now feel intolerable
support gaps feel stark
women see clearly how much they’ve carried
they realize how little they’ve received in return
resentment builds
This clarity is not cynicism; it is honesty. Midlife often brings the first real emotional inventory of a woman’s life — and it can be painful to see how much of herself she has given away.
5. The System Isn’t Failing — It’s Signalling
When women say they’re overwhelmed, depleted, or unable to keep up, they often assume they’ve changed in some unfortunate way.
But what’s really happening is that the body and mind are sending a message:
Something needs to shift.
The load was always heavy — but now the nervous system can no longer absorb the impact without consequences. This is not weakness. This is a legitimate call for rest, support, boundaries, redistribution of labour, or reevaluation of expectations.
The signal is not “you can’t cope.”
The signal is: “You shouldn’t have had to cope at this level for this long.”
6. There Is Nothing Wrong With You — There is something wrong with the load
Women are not burning out because they are fragile.
They are burning out because they are carrying too much.
Stress and emotional labour accumulate quietly over years, and perimenopause removes the internal scaffolding that made the weight seem manageable. This awakening can feel uncomfortable — but it can also be liberating. Many women begin, for the first time, to ask:
What do I actually want to carry?
What can I lay down?
What is mine, and what was never mine to hold?
What support do I deserve?
Where do I need boundaries?
Here is the point in midlife where honesty with ourselves meets biology — and it demands change.
The Role of Work & Culture
Most work environments were designed by men for men, and most definitely not perimenopausal women.
One of the most overlooked realities of perimenopause is how profoundly the outside world makes this transition harder. Women often assume their difficulty concentrating, coping, or managing emotional shifts reflects some personal inadequacy. But much of the suffering in midlife comes not from the biology itself, but from how poorly our external systems are designed to support women moving through it.
Workplaces, cultural expectations, and the distribution of emotional labour all converge at the exact moment women’s internal capacity is shifting. The result is a kind of friction — a mismatch between what the world expects and what the body is able to sustain.
Women describe this mismatch in remarkably similar ways:
“My workload hasn’t changed, but I’m exhausted in a way I’ve never been before.”
“No one at work understands what I’m going through.”
“Everyone still expects me to hold everything together.”
These aren’t complaints. They’re reflections of systems that were never built with women’s physiology in mind.
1. Workplaces Were Designed Around Bodies That Don’t Experience Menopause
Most modern work structures were created during eras when women were not present in the workforce — and certainly not in leadership roles. Expectations around productivity, attention, and emotional neutrality assume a steady internal state that simply isn’t realistic for someone navigating hormonal shifts, sleep fragmentation, heightened stress reactivity, or cognitive fluctuations.
This isn’t about weakness or incompetence. It’s about trying to meet unyielding expectations inside a body that is undergoing a natural, temporary recalibration. The structure doesn’t bend — so women are forced to. One in 10 women leave the workforce in Canada due to unmanaged symptoms of perimenopause.
2. Cultural Expectations Demand That Women Be Limitless
By midlife, many women are at the peak of their careers while also supporting aging parents, managing children or teens, maintaining homes, and absorbing the emotional tone of their relationships. Nothing in this cultural script accounts for a woman’s changing internal landscape. She is expected to continue functioning at full capacity, often without acknowledgment of what she’s quietly (or not so quietly!) enduring.
When women say they “can’t keep up,” it’s rarely because the demands increased. It’s because the culture around them refuses to adapt to a phase of life that half the population will experience.
3. The Pressure to Stay Silent Increases Emotional Strain
Because menopause has been treated as either a joke or a private inconvenience, many women feel they have no permission to speak honestly about their symptoms. They fear being dismissed, misunderstood, or perceived as less capable. So they push through, suppress their distress, and hope no one notices.
But emotional suppression is exhausting. Silence compounds stress. The fear of being seen as “less reliable” weighs heavily — especially on women who have built identities around competence and stability.
The result is a quiet, internalized struggle that intensifies symptoms that could have been eased with simple understanding or accommodation.
4. Western Culture Frames Menopause as Loss Rather Than Transition
In some cultures, menopause is associated with wisdom, increased authority, or a shift into a respected elder role. But in Western contexts, menopause is often portrayed as decline: a loss of fertility, femininity, desirability, and youth.
This narrative shapes how women interpret their own experience. Instead of seeing their anxiety, irritability, or cognitive changes as understandable consequences of hormonal transition, they see them as signs of aging poorly or losing value. This interpretation amplifies emotional suffering far beyond the biology itself.
5. The Burden Is Not the Woman — It’s the System
When you place a woman moving through hormonal transition into systems that demand linear productivity, constant emotional availability, and unwavering performance, of course she struggles. She is not designed to fail; the structure is designed not to accommodate.
The gap between what women actually need and what society expects creates a layer of distress that their physiology alone cannot explain. Women are not meant to be machines. They are living systems inside larger systems that are rigid, outdated, and unresponsive.
Midlife becomes difficult not because women are collapsing, but because the world around them refuses to acknowledge the reality of what their bodies are doing.
6. Understanding This Isn’t an Excuse — It’s Permission
When women realize that their struggles aren’t signs of personal inadequacy but reflections of structural limitations, something important shifts:
self-blame softens
boundaries feel more justifiable
rest becomes legitimate
advocacy feels possible
shame begins to loosen
The goal isn’t to lower expectations for women.
It’s to raise the standards of support around them.
Relationships & Menopause: Communication, Intimacy, and Changing Dynamics
Perimenopause doesn’t happen in isolation. It unfolds inside relationships — partnerships, marriages, friendships, family systems — and it inevitably reshapes them. Changes in mood, energy, sleep, identity, confidence, libido, and emotional bandwidth all ripple outward. For many women, this stage illuminates long-standing relational patterns that were once manageable but now feel unsustainable.
Women frequently say things like:
“I don’t feel as patient with my partner anymore.”
“We miscommunicate so easily now.”
“I love him, but I feel unseen.”
“I feel disconnected — from myself and from my relationship.”
“My needs are changing, and I don’t know how to talk about it.”
These aren’t relationship failures. They’re signs that internal change is exposing relational dynamics in need of attention.
Let’s explore how and why these shifts happen.
1. Emotional Bandwidth Shrinks — Communication Becomes Harder
When a woman’s nervous system becomes more reactive and her tolerance for stimulation decreases, communication that once felt effortless can suddenly feel draining. She may find it harder to articulate her needs, harder to manage conflict, or harder to stay emotionally regulated during difficult conversations.
Partners often misinterpret this as withdrawal or irritation. But it’s really the result of limited resources. When a woman is not sleeping well, managing anxiety spikes, or coping with cognitive changes, the emotional labour of explaining herself can feel overwhelming.
It’s not disconnection. It’s depletion.
2. Longstanding Relationship Patterns Rise to the Surface
Perimenopause is clarifying. Many women begin to see relational dynamics with sharper insight — especially dynamics that have been unequal, unbalanced, or emotionally one-sided. The tendency to appease, avoid conflict, or over-function becomes harder to maintain.
A woman who has carried the emotional weight of the household may suddenly find herself resenting it. A partner who avoids emotional conversations may feel even more distant. Patterns tolerated for years can start to feel suffocating now that internal resilience is shifting.
The friction is not new — the tolerance is.
3. Sexuality and Intimacy Change in Ways That Are Often Misunderstood
Sexual changes during perimenopause — whether decreased libido, increased sensitivity to overstimulation, discomfort, or emotional disconnection — are frequently misread as rejection. Partners may take it personally, and women often feel pressured to “explain” themselves when they barely understand the changes they’re experiencing.
Yet sexuality at midlife is profoundly complex. Confidence fluctuates. Desire becomes more tied to emotional safety and nervous system regulation. Women may crave closeness but feel less available for sex. They may want intimacy but not stimulation. Or they may experience a surprising increase in desire once irritability or anxiety is addressed.
None of these patterns are wrong. They are simply reflective of what the mind and body are undergoing.
4. The Relationship to Self Shifts First — and Everything Else Follows
Perhaps the most significant relational change is internal. As women reconnect with their needs, boundaries, preferences, and truth, the relationship they have with themselves becomes more central. They may feel drawn toward honesty, rest, solitude, self-reflection, or authenticity in ways they never have before.
This internal shift naturally affects every external relationship. Some deepen. Some realign. Some require renegotiation. And some cannot continue on the old terms.
Perimenopause often catalyzes conversations that were overdue — not because the woman is changing “too much,” but because she is finally becoming aligned with herself.
5. Partners Need Education, Not Guesswork
One of the biggest challenges is that many partners have no framework to understand what a woman is experiencing. They may only see the mood swings, irritability, forgetfulness, or withdrawal — without recognizing the complex hormonal and emotional foundation beneath.
When partners understand the physiology and psychology of perimenopause, something softens. Compassion increases. Defensive reactions decrease. Conversations become safer. The relationship becomes a place of support rather than pressure.
Midlife is not the end of connection — it’s a call for deeper understanding.
6. Change Doesn’t Mean Disconnection — It Means the Relationship Is Entering a New Chapter
Many women fear that the shifts they’re experiencing signal relational decline. But often, the opposite is true. Perimenopause exposes what needs attention so the relationship can evolve. It invites new agreements, clearer communication, shared responsibilities, and a more honest understanding of each person’s needs.
Relationships that weather this stage often emerge stronger — not because nothing changed, but because everything did, and both partners adapted.
7. What You’re Navigating Is Human, Not Personal Failure
If your relationship feels strained, tender, confusing, or reactive during this stage, you’re not alone — and you’re not doing anything wrong. Internal transition always affects relational dynamics. This stage asks for patience, honesty, vulnerability, and sometimes professional support.
You’re not too much. You’re not asking for too much.
You are moving through a transition that touches every layer of connection.
And you deserve a relationship that grows with you.
Self-Esteem, Body Image & Sexual Identity During Menopause
Perimenopause brings changes not only to mood, sleep, and cognition but also to how women see themselves — their bodies, their desirability, their sexuality, and their place in the world. These shifts can feel disorienting. They can stir grief, self-doubt, or insecurity, even in women who’ve spent years cultivating self-acceptance.
Women often tell me things like:
“I don’t recognize my body anymore.”
“I feel less confident — like something in me dimmed.”
“I don’t know where my sexuality fits now.”
“I want to feel good in my skin, but everything feels different.”
These changes are not superficial. They’re deeply intertwined with identity, relationships, and internalized cultural messages about aging, worth, and womanhood.
Let’s unpack the layers with care.
1. The Body Changes Faster Than the Identity Can Keep Up
Perimenopause can bring weight redistribution, changes in skin texture, bloating, shifts in muscle tone, thinning hair, or discomfort during sex. These changes happen during a stage of life when women are already carrying immense emotional labour and stress — which means there is little bandwidth left for adaptation or self-compassion.
The body no longer matches the familiar image a woman has held of herself, and identity often takes longer to adjust than appearance does. This lag creates a sense of disconnection: “This doesn’t feel like me.”
It’s not vanity. It’s the psychological work of integrating a new physical reality with a long-held internal narrative.
2. Women Are Navigating This Inside a Culture Obsessed With Youth
Western culture is relentlessly youth-centered. Women receive the message — directly (or indirectly - ha!) — that their value peaks in their 20s and 30s, and that aging must be resisted, solved, or concealed. When perimenopause brings visible changes, women often feel they are failing some unspoken standard.
The distress isn’t rooted in appearance — it’s rooted in cultural conditioning.
When women grieve how their bodies are changing, they are often grieving years of external pressure that taught them their worth was conditional. Understanding this softens shame, makes room for compassion, and gives context to feelings that might otherwise seem disproportionate and new.
3. Sexual Identity Often Feels in Flux
Sexuality in midlife becomes more complex. Some women experience a drop in libido; others feel desire that is more emotionally driven than before. Some feel disconnected from their bodies, and others discover a new, deeper connection with themselves.
These shifts aren’t random. Hormonal changes influence libido, but so do:
body image
energy levels
sleep quality
relationship dynamics
emotional safety
stress and burnout
how supported or unseen a woman feels in her daily life
Desire becomes less about spontaneity and more about what nurtures the nervous system. Women often want closeness, but not pressure; intimacy, but not overstimulation. Sexuality may change shape — but it doesn’t disappear. It evolves.
4. Old Narratives About Worth Resurface
Perimenopause often brings a resurgence of old insecurities — not because women are regressing, but because hormonal vulnerability magnifies sensitivities that were easier to suppress before.
Women who grew up with:
pressure to look a certain way
messages about “being attractive”
parental criticism about weight or appearance
partners who valued them for their beauty
internalized perfectionism
may find these wounds resurfacing with surprising intensity.
This is not a loss of confidence — it’s the nervous system activating old templates at a stage of biological change. When those templates appear, women often assume they’re “slipping backwards,” when in reality, they’re seeing the next layer of work with new clarity.
5. Grief and Self-Rediscovery Happen Side by Side
Menopause brings both loss and emergence. Women often move through grief — for youth, fertility, or predictability — while simultaneously experiencing a surprising expansion of identity.
Many women find themselves:
reconnecting with creativity
reclaiming autonomy
prioritizing authenticity
questioning old roles
deepening their sense of self
discovering sexuality on their own terms
feeling more grounded, direct, and self-assured
This duality can feel confusing. You can grieve one version of yourself while becoming another. Both experiences can coexist without conflict.
6. You Are Not Losing Yourself — You Are Relearning Yourself
Self-esteem in midlife isn’t about looking the same, feeling the same, or performing the same as you did in earlier decades. It’s about forming a relationship with a body and identity that are evolving, and making room for a more honest version of yourself — one that is less concerned with external expectations and more attuned to internal truth.
If you’ve lost confidence, it doesn’t mean your strength is gone. It means you’re in the process of recalibrating who you are in a body that is changing — and that recalibration is a normal, human, and deeply important part of midlife.
Grief, Loss & Life Transitions During Menopause
Perimenopause is not just a hormonal shift — it is a life stage marked by a constellation of transitions that carry profound emotional weight. Yet many women feel confused by the intensity of their feelings. They sense sadness, longing, or heaviness but struggle to identify the source. They say:
“I don’t know why I feel so emotional.”
“It’s like I’m grieving something I can’t name.”
“Nothing catastrophic happened, but I feel a deep sadness.”
“I feel like something is ending, and I didn’t choose it.”
These feelings make perfect sense. Menopause sits at the crossroads of multiple forms of loss — some concrete, some symbolic, some relational, some existential. And because our culture offers women little language for these quieter griefs, many carry them alone.
Let’s give shape to what so many women feel but rarely say.
1. Grief for the Body That Once Felt Familiar
The physical changes of perimenopause often bring a sense of losing the body you’ve known your whole adult life. Not just the appearance — but the reliability, the energy, the steadiness. Women grieve the body that could bounce back, the metabolism that felt predictable, the skin or hair that felt like “themselves,” the comfort they once felt in their own skin.
This grief is rarely talked about because it’s easily dismissed as vanity. But it’s not. It’s the grief of losing a familiar home — your own body — and learning to inhabit a new one.
2. Grief Related to Fertility — Even for Women Who Didn’t Want More Children
The end of the reproductive years can stir unexpected emotions. Even women who are certain they don’t want more children often feel a quiet sadness when the door fully closes. The loss is not necessarily about motherhood; it’s about the ending of a biological chapter, the passing of youth, or the realization that a certain version of the future is no longer possible.
It can feel like the body marking time in a way that the mind might not have been ready for yet.
3. Transitions Within Family Roles
Perimenopause often overlaps with children growing up, leaving home, becoming more independent, or entering stages that require less of a mother’s daily presence. Women may feel a sense of emptiness, disorientation, or longing as familiar rhythms shift.
At the same time, aging parents often begin to need more support. Women find themselves standing between generations, carrying the emotional weight of change on both ends.
This in-between place is tender — even when everything is “fine.”
4. Grief for Lost Versions of Yourself
Midlife brings a natural reevaluation of identity. Some women grieve the younger versions of themselves who felt freer, lighter, more hopeful, more energized, or more connected. Others mourn opportunities they didn’t take, careers they didn’t pursue, relationships they stayed in too long, or dreams they postponed until they quietly disappeared.
This is not rumination. It’s a normal period of reflection — a kind of life inventory that surfaces naturally in midlife.
Sometimes the sadness is simply about acknowledging, “I’m not her anymore.”
5. Loss in Relationships and Friendships
As women change internally, their relationships often shift too. Friendships may drift. Marriage dynamics evolve. Partners may not understand what a woman is experiencing. Long-standing patterns can no longer be maintained. The emotional landscape changes, and so do the people who inhabit it.
These changes can bring relief in some places and heartbreak in others. Both are normal.
6. The Existential Grief of Midlife
Perhaps the deepest layer is the existential one: the quiet awareness of time. A growing sense of life’s finiteness. A recognition that the future feels different than it did in earlier decades. A soft ache for what has passed, and an uncertainty about what comes next.
This is not depression — it is a developmental transition. A profound, often beautiful, confrontation with meaning.
Women aren’t breaking down when they feel this heaviness. They’re awakening to a new stage of life.
7. Grief and Growth Are Intertwined
Midlife grief is not something to “get over.” It’s something to move through — slowly, compassionately, with support. These feelings often create space for clarity, boundaries, self-reclamation, and renewed purpose. The grief softens when it’s acknowledged.
Women frequently emerge from this stage feeling more grounded, more aligned, and more connected to themselves than they’ve ever been.
Grief, in this sense, is a beginning.
Strength, Resilience & the Postmenopausal Brain: What Improves, Stabilizes, and Strengthens
For many women, perimenopause feels like a storm — unpredictable, exhausting, and emotionally destabilizing. It’s easy to assume that the turbulence is permanent, especially when sleep is disrupted, mood fluctuates, and cognitive changes appear without warning.
But research — and the lived experience of countless women — tells a different story.
Once the hormonal transition stabilizes and the nervous system no longer has to navigate extreme fluctuations, many women experience a surprising and profound sense of clarity, steadiness, and self-assurance. The body and brain adapt. The emotional landscape shifts. A period of life that felt chaotic slowly gives way to something much more grounded.
Let’s explore what strengthens in the postmenopausal years.
1. The Emotional System Regulates More Smoothly
When estrogen and progesterone stop fluctuating, the nervous system has a chance to recalibrate. Women often report fewer mood swings, a more consistent sense of wellbeing, and a steadier baseline. The unpredictability that characterized perimenopause gradually fades.
This doesn’t mean midlife stressors vanish — but your capacity to respond to them becomes more balanced and reliable again. Many women describe it as a return to themselves, or in some cases, meeting a more grounded version of themselves for the first time.
2. Cognitive Function Stabilizes — and Insight Deepens
While perimenopause can bring frustrating cognitive symptoms, these typically improve when hormone levels settle. Word retrieval becomes easier, mental fog lifts, and attention feels less scattered. The brain is no longer managing the constant internal noise of hormonal instability.
In addition to recovery of cognitive steadiness, there is often a deepening of wisdom and perspective. A woman’s ability to synthesize her life experience, make thoughtful decisions, and trust her intuition becomes one of her greatest strengths in this stage.
3. Confidence Often Increases Once the Turbulence Passes
With emotional steadiness returning, many women experience a notable rise in confidence. They feel less beholden to external expectations, less concerned with approval, and more anchored in their own values.
The identity work of midlife begins to show its benefits: clearer boundaries, stronger self-respect, and a sense of personal authority that isn’t as easily shaken as it may have been earlier in life. This confidence isn’t loud — it’s quiet, rooted, and deeply earned.
4. Women Become More Honest About Their Needs
The emotional vulnerability of perimenopause often brings clarity about what is no longer sustainable. Once on the other side, women are far less inclined to tolerate imbalances, over-functioning, unequal partnerships, or roles that diminish their wellbeing.
This honesty becomes a defining strength. Women begin to expect reciprocity, seek meaningful connection, and prioritize their health in ways they may have postponed for decades. Self-abandonment decreases; self-trust increases.
5. Relationships Can Become More Authentic
When a woman no longer expends so much energy managing symptoms or suppressing her needs, she has more capacity for genuine connection. Many relationships deepen as women communicate more openly, invite shared responsibility, and allow themselves to be supported.
Other relationships, especially those that relied on her over-functioning, may shift — sometimes dramatically. While this can be challenging, it often leads to healthier, more authentic relational patterns.
Postmenopause becomes a time of relational honesty, not withdrawal.
6. A Sense of Freedom Often Emerges — Sometimes Unexpectedly
With the reproductive years behind them and identity expanded beyond society’s narrow expectations, many women feel a sense of liberation. Freed from monthly fluctuations, fertility concerns, or the emotional weight of constant prioritization, they step into a phase defined not by survival, but by intention.
Women describe feeling:
less apologetic
less pressured
less self-critical
more curious
more grounded
more themselves
This freedom isn’t about circumstance; it’s about internal alignment. It’s a shift into a life shaped by truth rather than habit.
7. You Are Not Moving Toward Decline — You Are Moving Toward Stability
Despite cultural narratives that frame menopause as loss, many aspects of physical, emotional, and cognitive wellbeing actually improve once the transition is complete. The storm quietens. The internal landscape becomes clearer. The system regains its equilibrium.
Postmenopause is not the shrinking of a woman’s world — it’s an opportunity for expansion, authenticity, and a renewed connection to self.
You are not fading.
You are emerging into a more anchored, stable, and powerful version of yourself.
How Partners, Families, and Communities can Support Women Through this Transition
Perimenopause is a deeply personal experience, but it’s not one meant to be endured alone. The women who navigate this transition with support — emotional, practical, relational, and professional — often find the journey far more manageable. Yet most of the people around them have little understanding of what is happening internally. They see the exhaustion, irritability, forgetfulness, or overwhelm, but not the physiological and emotional complexity beneath it.
Women often tell me, “I wish the people in my life understood this better.”
They don’t want pity. They want to be seen.
Let’s explore how support actually works during this transition — not as a list of tasks, but as a shift in understanding, expectation, and connection.
1. Understanding Makes Everything Easier
Partners and family members don’t need to become menopause experts — but they do need a framework. When they understand that perimenopause affects sleep, mood regulation, cognitive function, stress tolerance, and emotional bandwidth, they stop personalizing a woman’s reactions and start recognizing the underlying process.
This shift alone softens defensiveness, reduces conflict, and makes room for empathy. It changes the question from “What’s wrong with her?” to “What is she navigating right now?”
Understanding is a form of love.
2. Emotional Safety Matters More Than Solutions
Many women in perimenopause don’t need someone to fix anything — they need someone to sit with them, listen without rushing, and acknowledge that what they’re facing is hard. This isn’t fragility; it’s the need for attunement during a time when internal resources are stretched thin.
Support sounds like:
“I hear you.”
“You’re not alone.”
“I didn’t realize how much you were carrying.”
“How can I make things easier right now?”
Emotional safety is not passive. It’s a deliberate choice to meet a woman where she is, rather than asking her to meet others’ expectations.
3. Sharing the Load Is Not Optional — It’s Necessary
When a woman’s sleep, mood, and stress tolerance are impacted, carrying the full weight of household labour, childcare coordination, emotional caretaking, or social organizing becomes unsustainable. Redistributing the load is not an act of charity — it’s an act of partnership.
Sometimes this looks like taking on practical tasks. More often, it looks like quietly assuming responsibility without being asked, noticing what needs attention, stepping into discomfort, or shouldering emotional labour that a woman has carried alone for years.
This is where relationships deepen — not through grand gestures, but through consistent contribution.
4. Loved Ones Can Support the Nervous System
Support is often most effective when directed toward helping a woman feel regulated, not pressured. Partners can help by creating a calmer environment, reducing unnecessary stimulation, and being patient during moments when she is overwhelmed or overstimulated.
This is not coddling. It is co-regulation — one of the most powerful forms of emotional support humans offer each other.
Small moments of steadiness from others act as anchors during a time when the internal landscape feels unpredictable.
5. Friendships Become Lifelines
Connection with other women — especially those going through similar transitions — often becomes incredibly grounding. These friendships offer validation, humour, shared wisdom, and an emotional shorthand that reduces isolation.
Women feel less alone when they realize, “Oh, it’s not just me.”
Sharing stories normalizes the experience.
Normalizing the experience reduces shame.
Reduced shame bolsters emotional capacity.
Think of friendship is as nourishment during this stage.
6. Community and Culture Play a Role
When workplaces, families, and communities normalize conversations about menopause, women feel less pressure to hide their symptoms or push through distress silently. They are more likely to seek help, set boundaries, and ask for what they need.
A woman’s transition becomes easier not just because her biology stabilizes, but because the ecosystem around her becomes safer and more responsive.
We can’t change all systems, but we can create pockets of understanding — and those pockets matter.
7. Support Doesn’t Have to Be Perfect — It Has to Be Present
Partners, family, and friends don’t need to know exactly what to do. They just need to show up with consistency, curiosity, and compassion. They need to believe women when they describe what’s happening inside their bodies and minds. They need to trust women’s lived experience, even when it challenges their assumptions.
Women are not asking for miracles.
They’re asking for recognition.
For partnership.
For attunement.
For rest.
Support in midlife is not about doing more — it’s about being more aware, more humane, and more willing to adapt together.
A Closing Note: You Are Not Meant to Navigate This Alone
If you’ve read this far, you’ve probably recognized pieces of yourself — the overwhelm, the irritability, the fog, the questions about identity, the grief, the fatigue, the sudden clarity, the emotional reactivity, the longing for support, the sense of becoming someone new while trying to hold together the life of the woman you once were.
Perimenopause is not a small chapter in a woman’s life.
It is a full landscape — one that reshapes your body, your brain, your relationships, your energy, your boundaries, your values, and your sense of who you are in the world.
And because this transition is rarely acknowledged — let alone explained — too many women move through it silently, believing they are failing, falling apart, or somehow “not themselves” anymore. But nothing in this transition is a personal flaw. It is a biological, emotional, psychological, and social turning point.
If no one has said this to you yet, let me say it here:
You are not doing anything wrong.
You are not losing yourself.
You are adapting to a profound change with courage and integrity — even when it doesn’t feel like it.
The turbulence of midlife is temporary, but the insight you gain from it is lasting. The clarity that emerges. The honesty. The boundaries. The reclamation of self. Women often describe the other side of this transition as a return to themselves — or, more accurately, a return to a self they never had the freedom to be before.
You are not shrinking.
You are emerging.
As you move through this stage, you deserve informed care, thoughtful guidance, emotional support, and spaces where your experience is taken seriously. You deserve people who understand that this is not merely “hormones,” but a complex interplay of biology, identity, history, and responsibility. And you deserve tools that help you navigate the hardest moments with compassion rather than pressure.
This guide is a starting place — a map of the terrain.
But you do not need to walk it alone.
If you see yourself in these pages, know that support exists.
Understanding exists.
Relief exists.
A steadier future exists.
Most importantly:
You exist — whole, worthy, and evolving — throughout every stage of this transition.
Welcome to the next chapter.
You get to write it on your terms.